Tooth extractions are sometimes unavoidable—whether it’s decay, infection, or overcrowding. Once it’s out, pain relief becomes the priority. But before you reach for ibuprofen, you might want to consider the complications.
Most people experience some discomfort or post-extraction pain. Unless you develop dry socket, the pain usually subsides within a few days. Your dentist or oral surgeon will commonly prescribe painkillers to manage this discomfort.

Ibuprofen is a popular over-the-counter (OTC) pain medication. However, some dentists advise against its use after a tooth extraction. Why no ibuprofen after a tooth extraction? And what should you take instead?
Why You Shouldn’t Take Ibuprofen After a Tooth Extraction
Ibuprofen is the gold standard for pain relief. Although technically an anti-inflammatory, ibuprofen also offers strong pain-relieving effects. Little wonder it’s one of the most commonly used medications in the world.
So, why the caution post-extraction?
Ibuprofen carries several risks that can occur after a tooth extraction. These include:
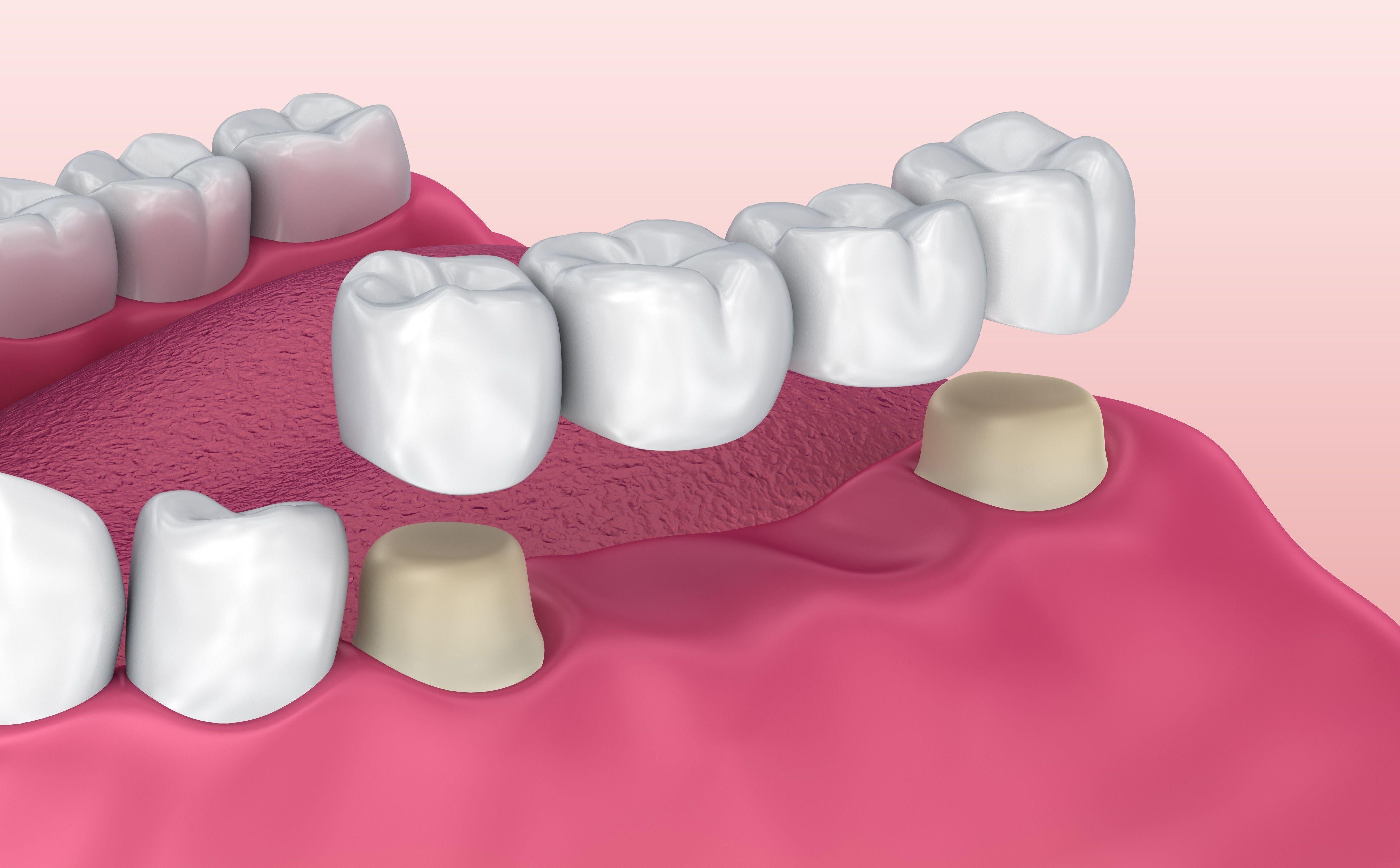
· Increased risk of bleeding. Ibuprofen has a minor blood-thinning effect. While it’s not as potent as aspirin, it can lower the chance that a blood clot forms in the socket. This is a crucial step in the healing process. The blood clot protects the underlying gums and exposed nerves, preventing dry socket – an extremely painful condition.
· Delayed healing process. Inflammation is a natural part of the body’s healing process. If ibuprofen disrupts inflammation, it can prevent the body from clearing out damaged cells and bacteria at the wound site. It might cause a little more pain in the short term, but long-term, it increases the chance of better results.
· Gastrointestinal issues. One of the most common side effects of NSAIDs is gastrointestinal disruption. These medications can increase the risk of GI bleeding, especially in patients who aren’t eating. Given that a tooth extraction might lower your appetite, it’s not the best option.
These issues might not sound like a big deal. The main risk is the development of dry socket. This condition occurs when a clot fails to form or is dislodged, leading to a week or more of deep, aggravating pain.
How Does Ibuprofen Work?
Ibuprofen is primarily an anti-inflammatory with some analgesic effects. It works by inhibiting two enzymes called COX-1 and COX-2. These enzymes produce prostaglandins, which cause your blood vessels to relax and widen, help platelets form blood clots, and increase inflammation in your tissues.
By inhibiting these enzymes, ibuprofen effectively prevents these actions.
Ibuprofen also has an analgesic effect. Fewer prostaglandins relieve inflammation and swelling, helping to soothe any pain.
As you can see, it’s the very action that reduces pain and inflammation that presents the greatest risk to patients’ post-extraction.
Adverse Effects of Ibuprofen
Ibuprofen is extremely well-tolerated in most people. The chance of side effects is relatively low, in part because most people only take ibuprofen for a few days at a time.
However, if people take ibuprofen in large doses or for prolonged periods, the risk of GI bleeding increases significantly. Concerning signs include:
· Black stool or blood in your vomit – these are characteristic signs of bleeding in your stomach.
· Swollen ankles, blood in your urine, or not urinating at all – this is a sign of a kidney problem.
These adverse effects are rare. More commonly, people may experience:
· Headaches
· Dizziness
· Nausea and vomiting
· Indigestion
· Flatulence
If you experience any of these side effects, lower your dose or stop taking ibuprofen. It’s important to drink plenty of fluids and to rest. Avoid eating any rich or spicy food that may exacerbate stomach discomfort.
Why Ibuprofen Is Safe After Extraction
Not all extractions are the same. In minor or routine cases where healing is progressing well, the clot has already formed, and the patient isn’t at high risk of bleeding, dentists may approve short-term ibuprofen use.
In some cases, ibuprofen is the best option after the initial 24-48 hours, so long as the clot remains stable. The risk of dry socket continues to fall as time goes by, lowering the risk from ibuprofen.
For example, if you’ve had a simple extraction (non-wisdom tooth) with no complications and you’re not on any blood-thinning medication, ibuprofen is an excellent painkiller. We recommend speaking to your dentist before taking it.
What Painkillers Can You Take?
Ibuprofen isn’t the only painkiller available. If you cannot take ibuprofen or your dentist advises against it, you can consider:
· Paracetamol (acetaminophen). Just as effective as ibuprofen, paracetamol is a popular option for pain relief. It has a similar mechanism of action but doesn’t interfere with the clotting process or cause GI issues. Therefore, it’s completely safe for patients after a tooth extraction.
· Prescription medication. If your pain is severe, your dentist may prescribe a stronger pain reliever, such as opioids. These are perfect for short-term pain relief. However, there is a risk of dependency. Other side effects include constipation, nausea, and confusion.
· Natural remedies. Several non-pharmaceutical remedies can relieve dental pain. Applying a cold compress to the outside of your cheek can soothe inflammation, numb the area, and provide temporary pain relief. A saltwater rinse is also advised to clean the extraction site and reduce the risk of infection. Lastly, clove oil is sometimes applied to the extraction site to numb the pain.
Ibuprofen vs Paracetamol After Extraction
Unless your dentist says otherwise, most people have a choice between ibuprofen and paracetamol. You can take both – in fact, a combination approach provides the greatest level of pain relief. However, patients usually opt for one or the other.
Let’s compare each:
|
Painkiller |
Benefits |
Risks |
Suitable Post-Extraction? |
|
Ibuprofen |
Strong anti-inflammatory and pain relief |
Inhibits clotting, may delay healing, GI issues |
Not advised in early stages |
|
Paracetamol |
Gentle on stomach, safe for most |
Less anti-inflammatory action |
Safe and widely recommended |
Generally, it’s better to rely on paracetamol for the first few days following extraction. This gives the clot time to form. If you’re still feeling any minor discomfort after a few days, it may be safe to introduce or switch to ibuprofen.
That being said, if you continue to experience pain for several days post-extraction – and the pain does not subside – seek medical attention. It might be a sign of infection or dry socket.
Why Tooth Extraction Aftercare Matters
Tooth extraction aftercare isn’t an afterthought – it’s the difference between a successful recovery and pain and complications. Here are some potential risks:
Dry Socket
Dry socket occurs when the blood clot protecting the exposed extraction site either never forms or becomes dislodged. The site begins to dry up, becoming extremely painful. This pain is distinct from the typical kind of pain associated with an extraction.
Usually, it begins within 1 to 3 days after your tooth is pulled out. It can persist for a week or more and is difficult to treat. Other associated symptoms include:
· Intense pain within the first few days after the extraction
· Pain spreading from the socket to your ear, eye, or neck
· A missing or dislodged blood clot at the extraction site
· Unpleasant taste in your mouth
· Persistent bad breath
· Mild fever
Ibuprofen is one risk factor for dry socket. However, it can also be caused by smoking or vaping, poor oral hygiene, diabetes, chemotherapy, age (peak incidence between 18 and 33 years), and use of oral contraceptives.
Dry socket occurs in around 1-3% of tooth extractions, rising to almost a third in wisdom tooth extractions.
Other Complications
Delayed healing and infection are the other main complications. Ibuprofen is a vasoconstrictor, so it decreases blood flow to the extraction site. This prevents white blood cells from reaching the site and fighting an infection.
Conversely, the reduction in prostaglandins stalls the body’s inflammatory response. Inflammation may feel uncomfortable for patients; however, it’s a critical step in the body’s immune defence. Without inflammation, the site can experience slower healing and an increased risk of a severe infection.
Tips for Tooth Extraction Aftercare
Want to avoid any complications? Follow these steps:
· Wash with a saline solution. Gently swill your mouth with saltwater to kill any bacteria and disinfect the extraction site.
· Use a sonic toothbrush. You can continue to use your sonic toothbrush. Be careful to avoid the extraction site. Always leave it 24-48 hours before you resume brushing. Opt for a soft-bristled head to ensure it’s not too abrasive and resume brushing gradually.
· Opt for a soft diet. Eating chewy or sticky foods increases the risk of dislodging the clot. Choose easy-to-eat, soft foods that aren’t going to cause any major issues.
If you’re using an Oclean sonic toothbrush, switch to the sensitive gum care mode during recovery and avoid brushing the extraction site. The Oclean X Pro Sonic Toothbrush, powered by a Maglev motor, helps drive toothpaste between teeth and along the gumline—reducing plaque, decay, and gum disease so you can avoid extractions in the first place.
Table of Contents